Why is Single Embryo Transfer Used?
Since the early years of in vitro fertilization (IVF) the chance of each embryo producing a baby has increased markedly. In decades past multiple embryos were transferred back to the uterus in hopes that at least one would implant. The problem was that there was no way to know if just one or if all embryos would implant. This has led to the well documented link between IVF and multiple pregnancy, whether its twins, triplets or more. As available technologies have improved and IVF has become more efficient, the American Society of Reproductive Medicine (ASRM) has started recommending guidelines for the number of embryos transferred in order to maximize your chances of having a healthy pregnancy. At RMA New York a combination of expert laboratory techniques and advanced diagnostic technologies are utilized to select the embryo that will give the best chance of producing a healthy baby and preferentially transferring that embryo.
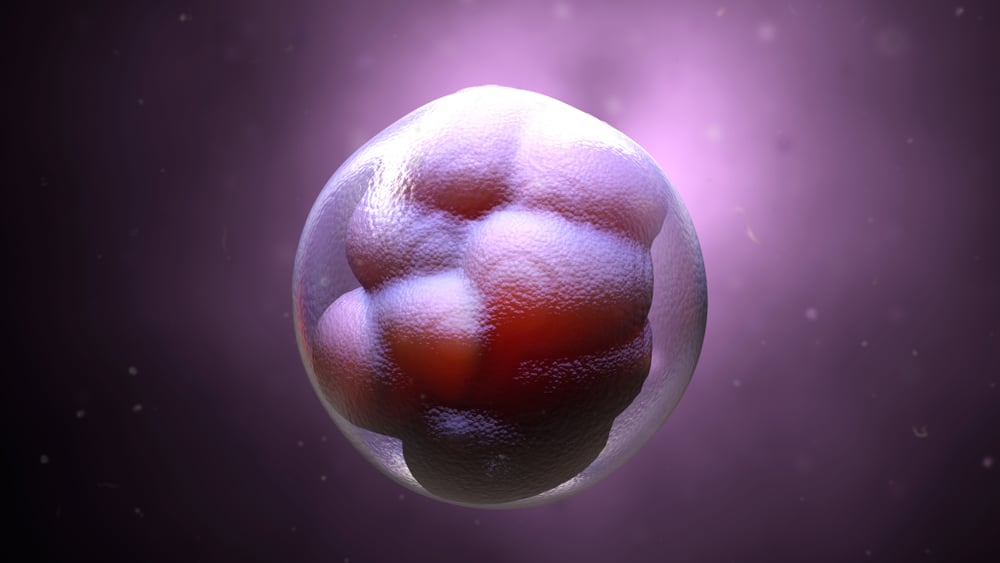
The first major advancement in embryo selection came when growing embryos for longer before replacing them to the uterus became possible. This is called extended embryo culture and allows you to see which of the embryos that are growing after 2 or 3 days will make it to a healthy embryo on day 5 or 6, known as a blastocyst. The embryos that grow to day 5 or 6 have a higher chance of producing a healthy baby and so you can transfer one of them as opposed to multiple embryos from day 2 or 3 of culture without sacrificing pregnancy rates. Information regarding embryo morphokintetics is used to further identify which blastocysts have the highest implantation potential. In this process the speed at which the embryo develops and the appearance of cells that make up the blastocyst are all used to select the best embryo to transfer.
Another tool to help you select the best embryo to transfer is preimplantation genetic testing (PGT) using the newest DNA sequencing technologies (next generation sequencing) to identify which embryo has the correct number of chromosomes and focusing your energy on that embryo. This can be used in conjunction with morphokinetics to optimize embryo selection. In fact, ASRM recommends that you only transfer onein all patients with genetically screened chromosomally normal embryos.
Finally, advancements in embryo freezing, through a process known as vitrification, allow you to store your embryos for future use without sacrificing, and maybe even improving, your pregnancy rates after embryo transfer. This allows you to transfer one embryo at a time and know that the remaining embryos will be there waiting if and when they are needed. In fact, data is clear that transferring 2 embryos one at a time gives you a higher overall pregnancy rate than transferring 2 at once while dramatically decreasing the chance of a multiple pregnancy.
Pregnancy with twins or more is a high risk pregnancy that leads to significantly more complications for mom and babies. For mom there is an increased risk of blood pressure disease (pre-eclampsia), diabetes, c-section, and dangerous hemorrhage at the time of birth. For babies there is an increased risk of premature birth, poor growth, cerebral palsy and developmental delays. By optimizing embryo selection and embryo freezing techniques you can feel confident transferring one embryo at a time. This will allow you to increase your chances of getting pregnant while also maximizing the chance that the pregnancy will result in a healthy mom and healthy baby.
