IUI vs. IVF: What's the Difference?
Couples who are having difficulty conceiving may wonder if they should undergo fertility treatments and what type of treatments should be considered. Two procedures commonly used to help couples are intrauterine insemination (IUI) and in vitro fertilization (IVF). There are key differences between IUI and IVF treatment. Comparing both options can help you determine which approach might be best for you and your partner.
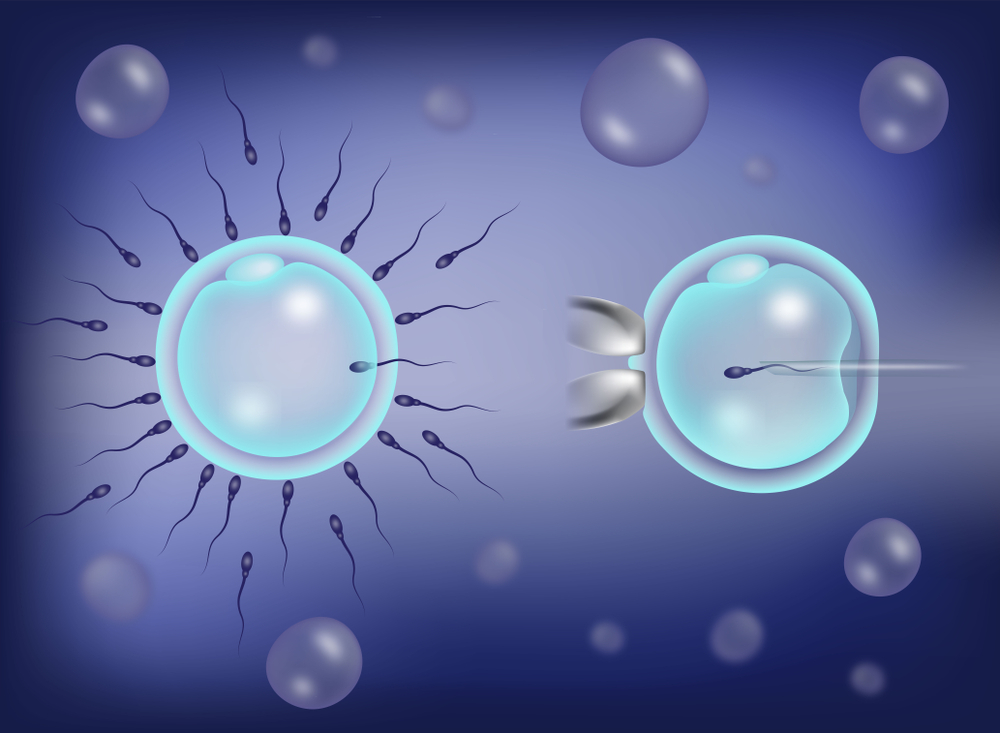
Couples with infertility often start treatment with IUI, which is much less invasive than IVF. IUI involves placing a washed sperm directly into the woman’s uterus during the fertile window. This can be done as part of a natural cycle or, more often, in combination with medications (like clomiphene citrate or letrozole). The washed sperm sample will contain more motile sperm, which are more likely to fertilize an egg. Additionally, placing sperm directly into the uterus means they do not need to “swim” as far to reach their target.
The decision to proceed with IUI instead of moving directly to IVF is based on diagnosis and sperm count. A basic element of a fertility evaluation is the semen analysis. A specimen produced after 2-3 days of abstinence may be evaluated (among other things) for count, motility and morphology. Typically the sperm count should be greater than 10 million per milliliter, at least 40% of the sperm should be moving properly, and at least 4% of sperm should be normal in shape (morphology using Kruger strict criteria). If the total motile count is less than 1 million, IVF should be considered. Also, if morphology (this describes the ability of sperm to bind eggs) is less than 4% IUI should be considered.
In addition to helping couples with mild to moderate male factor infertility, IUI can be useful for couples who are having trouble conceiving for other reasons, such as their work or travel schedule, sexual dysfunction, unexplained infertility or various other fertility conditions.
Reasons to Pursue IVF
IUI can be a good starting point for couples facing issues involving ovulation or unexplained infertility. However, IUI may not be the most suitable fertility treatment for a couple. IVF is usually recommended for couples facing the following situations: severe male infertility, damaged fallopian tubes, lack of success after 3-4 IUI attempts, or concern about transmitting genetic disorders.
IVF allows more directed therapy of fertility issues by improving conditions for fertilization, optimizing the environment for embryo development and placing embryos directly into the uterus, bypassing potential issues in the fallopian tube. IVF typically is accomplished with a ten day course of fertility medications that permit multiple eggs to mature. Blood testing and ultrasonography are used to monitor progress of egg growth until optimal development is determined. These eggs are then collected thru a minor procedure utilizing a needle to harvest mature eggs. Subsequently, embryos are developed outside the body in the IVF laboratory until growth and testing are completed. A single embryo is then placed into the uterus under ultrasound guidance.
Pre-implantation genetic testing is an advanced scientific procedure that can be performed before IVF. This may be beneficial for patients who have concerns about a genetic condition or who have had multiple unsuccessful IUI cycles or miscarriages. This procedure can be used to identify genetic disorders or chromosomal abnormalities in embryos, and can help identify the best embryo to transfer.
Both IUI and IVF play an important role in fertility therapy. IUIs are helpful in many cases of infertility but IVF may be necessary in more complicated or longstanding fertility cases.
