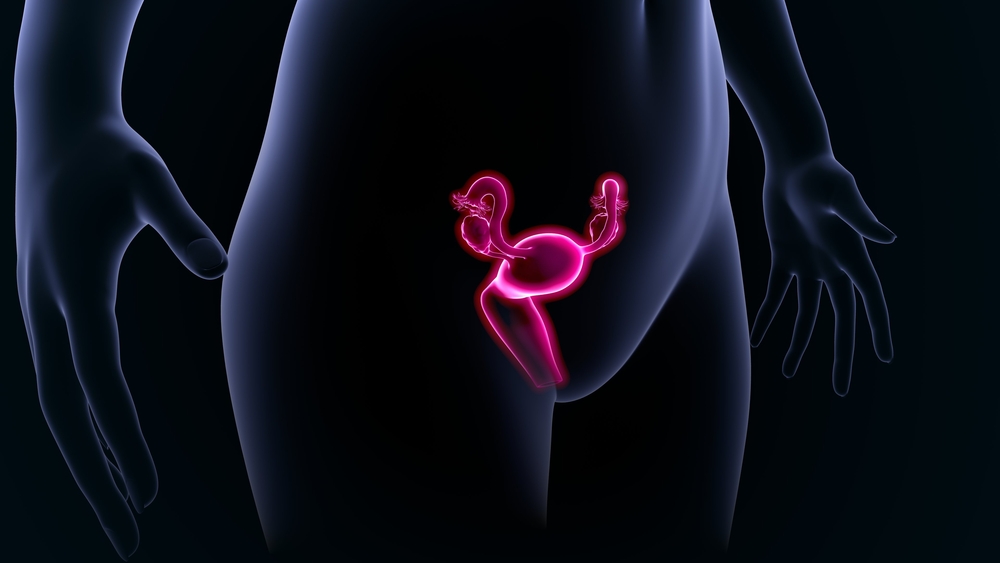
Female Reproduction 101
The biology of the female reproductive system is of particular interest to women and couples who are interested in conceiving. A woman’s ovaries play an important role beyond reproduction in hormone production, as estrogen is critical in maintaining bone health and preventing osteoporosis, along with other health benefits.
For a pregnancy to occur, a mature egg must be fertilized by sperm. This fertilized egg, now called an embryo, then implants in the uterus. Fertilization typically takes place in the fallopian tubes, which connect the uterus to the pelvis where the ovaries reside. In a typical menstrual cycle, an egg starts to mature in the ovary, in fluid filled structures called follicles. While eggs are microscopic, follicles can readily be viewed by ultrasound. The number of follicles visible on ultrasound give insight into a woman’s egg number, also called ovarian reserve. In a typical cycle, one egg fully matures, with the corresponding follicle increasing in size dramatically, while other eggs that have begun to mature arrest and die off – a process called atresia. The egg maturation process, starting early in a menstrual cycle shortly after a period, is driven by the hypothalamus which rests in the base of the brain. The hypothalamus produces a hormone called gonadotropin releasing hormone (GnRH), which in turn drives the pituitary gland that resides nearby connected by a stalk to produce follicle stimulating hormone (FSH). Around mid-cycle when the follicle and egg are mature, a second hormone is produced in high quantity by the pituitary called luteinizing hormone (LH). This surge in LH induces the final maturation of the egg and ovulation where rupture of the follicle and release of the egg into the pelvis occurs. The fallopian tube, in turn, sweeps over and picks up the egg which is then carried into the tube where it can be fertilized if there are sperm residing in the tube.
After ovulation, hormone production by the ovary changes from primarily estrogen production from the maturing follicle to estrogen and progesterone production from the now ruptured follicle which transforms into a structure called a corpus luteum. Progesterone acts on the lining of the uterus, which had been thickening in response to estrogen from the maturing folllicle, to induce final changes in the lining to make it receptive to an embryo. If the egg fertilizes normally, the embryo generally makes its way into the uterus a few days later. Once in the uterus, the embryo can then implant in the uterus. In order to sustain a pregnancy ongoing estrogen and progesterone production form the ovary is critical. Pregnancy hormone (human chorionic gonadotropin or hCG) is important to maintain the corpus luteum which continues estrogen and progesterone production to support the pregnancy until the placenta can take over hormone production at about 8 weeks gestation (counted from the first day of a menstrual period). If no pregnancy ensues, then the corpus luteum regresses and declining hormone production causes the lining of the uterus to break down and results in menstrual bleeding.
Several points are worth noting when it comes to female reproduction. Unlike sperm, which are produced every 3 months or so, a woman is born with all the eggs she will have. This number is estimated to be about a million at birth, with egg numbers approaching 400 thousand at the time of puberty. It is also important to note that in the course of a month, while generally one egg matures and ovulates, many more eggs die off from atresia. Oral contraceptives, which prevent eggs from maturing, do not retard the rate of egg decline as those same cohort of eggs will become atretic. Conversely, women who take fertility medications don’t lose more eggs each month, but rather eggs that would otherwise become atretic and die off are rescued and will fully mature. So women on contraceptives do not preserve eggs and go through menopause later. Conversely, women who have taken fertility drugs do not lose eggs at an accelerated rate and go through menopause earlier. The age at which a women enters menopause, when most eggs have been already released, varies considerably with an average age of 51. The rate of egg decline also varies greatly between women. This rate also has been shown to accelerate at some point in a woman’s lifetime, and the age at which this accelerated rate of decline occurs also can vary. Any assessment of ovarian reserve is thus a current snapshot in time, and while changes rarely occur in a few short months, the variability in rate of egg loss does make projections of future ovarian reserve difficult.
It also bears mentioning that the reproductive capacity of the uterus does not change over time. Women with low reserve or even those who have entered menopause are able to respond to estrogen and progesterone and carry a pregnancy. This enables one to use a donor egg at more advanced reproductive ages with a high likelihood of success.
