Commonly Asked IVF Questions
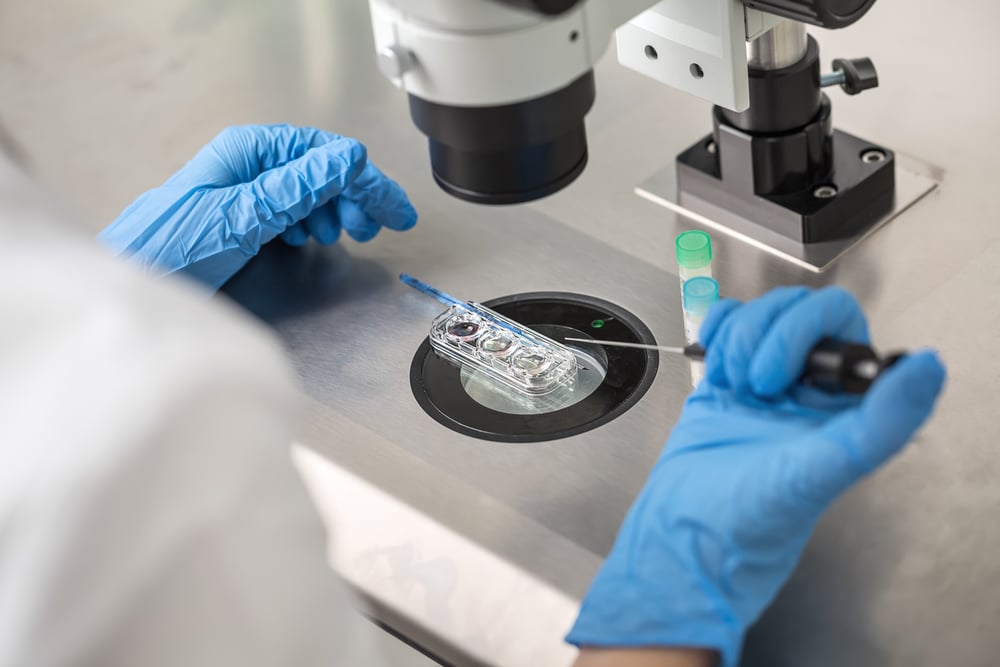
IVF, the most commonly performed assisted reproductive technology (ART), is used worldwide by patients and couples trying to conceive. As a reproductive and infertility specialist, I answer IVF questions from patients daily, and decided to compile some of the more commonly asked IVF questions I receive.
IVF or In Vitro Fertilization is a procedure in which multiple eggs are stimulated to mature and are then retrieved. The egg retrieval process is usually done under light anesthesia and takes about 10 to 15 minutes to perform using a needle under ultrasound guidance. No incisions are required and so the recovery is typically fairly easy with mild bleeding and cramping being the most common symptoms post retrieval, and most patients able to return to their normal routine the following day. Eggs can then be frozen for patient interested in fertility preservation, or fertilized to create embryos that can then be used to help a woman or couple conceive.
How long is the IVF process from start to finish?
It typically takes 2-4 weeks to prepare for IVF, and the stimulation phase entails about 8-10 days of fertility shots and an egg retrieval is performed 2 days later.
Is IVF painful?
Most patients do not report significant discomfort during the IVF process. Some women may feel bloating during the ovarian stimulation phase, and light bleeding or cramping may occur after egg retrieval.
What are the potential side effects of undergoing IVF?
Given streamlined changes in the process, most patients tolerate the process really well. We rarely see ovarian hyperstimulation these days, since we changed our medication protocols. Since we use sequencing technologies to identify healthy embryos, we can now avoid twins and triplets. In other words, aside from bloating and inconvenience, IVF is now really well tolerated.
Is there anything that could negatively impact IVF success?
Given the decline in egg quality that occurs with age, women who are older or who experience premature ovarian aging often take more attempts to produce a healthy egg. By maintaining a healthy life style, a healthy body weight, and a focus on health and wellness, success rates can be optimized.
Where are eggs/sperm/embryos stored?
At RMA of New York, gametes and embryos are stored in our andrology and embryology laboratories. Eggs, sperm, and embryos are stored in liquid nitrogen. The duration of time gametes and embryos are frozen does not affect the success rate of the procedure using the frozen specimen. At RMA of New York all frozen specimens are located on-site in a secure room equipped with a 24-hour-a-day, 7-day-a-week alarm-monitoring system to alert embryologists regarding any change in temperature.
What does Day 3/5/7 transfer mean?
Historically, embryos were transferred after 3 days post retrieval, because our ability to culture embryos beyond this point wasn’t efficient. Today, given advances in culture techniques and clean room technology, most top centers are able to culture until the blastocyst stage (day 5-7). Extended culture enables us to better select embryos for transfe,r as they are at a more advanced stage of development. An additional benefit of extending culture to the blastocyst stage is that placental cells (trophectoderm) can be biopsied and analyzed, allowing us to confirm that the healthiest embryos are the ones selected for transfer.
Does the process change if using donor eggs or sperm?
No, IVF can be used with donor sperm – which freezes and thaws well – or a patient can opt to use an egg donor if necessary for a successful outcome.
Will I lose eggs faster if I take fertility drugs that result in multiple eggs ovulating and releasing each month?
No. Women lose the same number of eggs each month regardless of any medications that alter how many fully mature and ovulate (or are retrieved during an IVF cycle). Fertility drugs rescue more eggs that are destined to die off (called atresia) that month. Incidentally the converse also holds in that oral contraceptive use, which prevents an egg from ovulating altogether, doesn’t protect eggs from being lost each month. Use of fertility drugs and oral contraceptives don’t affect the age at which a woman will reach menopause (when eggs have been depleted).
Why is it necessary to have so many eggs while undergoing IVF?
The human reproductive process is inherently inefficient. Some eggs are immature. Some mature eggs won’t fertilize normally. A proportion of embryos arrest – presumably due to some inherent abnormality in the embryo. A proportion of embryos that do well in culture are genetically abnormal. So while the number of eggs necessary to achieve a live birth depends in part on a woman’s age, the fact remains that in all women most eggs will not lead to live births. Also, importantly, extra embryos can be frozen for future use. This enables more than one attempt at pregnancy per egg retrieval in many cases, and more than one child from one retrieval cycle if extra embryos are available for cryopreservation.
