A Fertility Journey Through the Eyes of a Young Previvor: Honoring National Cancer Prevention Month
At the age of 22, I heard the words, “You have your mother’s BRCA1 mutation.” My world flipped upside down that day. I was referred to a slew of doctors, and almost all of them asked me what my goals were for family planning considering the screening and surgery decisions I would have to make. At the time, I had no clear picture of being settled and I wasn’t in a relationship in which I felt comfortable bringing kids into my life. In addition, I couldn’t comprehend having a child naturally, knowing that there was a 50/50 chance that they would inherit my BRCA mutation. For many years, I lost the dream of one day being a mother—it seemed impossible.
About five years later, I was in a long-term, committed relationship and pursuing therapy at the Duke Cancer Center. Upon hearing that I told myself I could never have children, my therapist encouraged me to reach out to a provider at the Duke Fertility Center to discuss my options. I was extremely nervous about this appointment, fearing that my thoughts would be confirmed: I would never have a chance at motherhood.
The outcome was opposite to what I expected. The reproductive endocrinologist confirmed that no matter the circumstance, I would be able to bring a child into this world knowing that they would not carry my mutation.
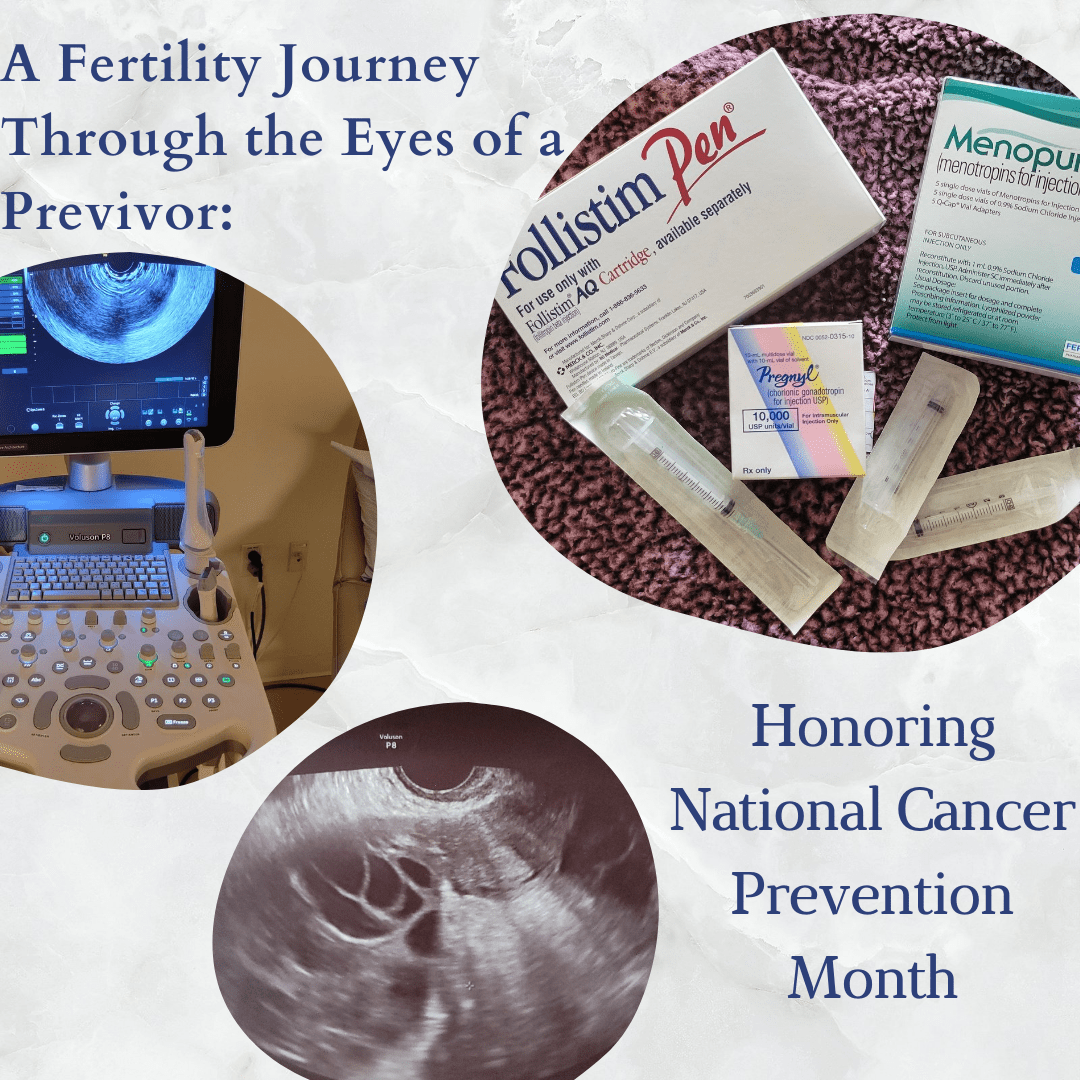
The process for doing this is called pre-implantation genetic diagnosis (PGD). A reproductive endocrinologist would retrieve my eggs and my partner would donate a sperm sample, which they would then use to fertilize my eggs. Once viable embryos formed from those fertilized eggs, they would take a few cells and send them for genetic testing to see if they carried my mutation. I could still have a viable pregnancy even if I decided to have my ovaries removed before having a child. I was shocked and so excited that motherhood could be an option for me.
At the time, however, I was not ready to pursue this. My partner and I were not yet married and I wanted to pursue frozen embryos versus frozen eggs, as my reproductive endocrinologist said this would be the most successful option. The other reason was that this process is insanely expensive, I was reassured that they had a financial counselor who could help me with medical loan programs and pharmacy programs to help afford the medication I would need to trigger the release of hormones that would stimulate egg production and maturation.
My husband and I were married in December 2019. Then, in March 2020, the whole world fell apart. It felt like this dream was never going to happen for me. I was in the process of planning my risk-reducing bilateral mastectomy with the hope of doing a round of IVF treatments afterward. I heard horror stories of surgeries and embryo transfers being delayed because of COVID precautions. It took several months for me to finally book my mastectomy and find a provider for IVF treatments.
I had my mastectomy in August 2020, and the following March we finally started the IVF process. The experience was tougher than I had anticipated. The shots those first few days were a little painful, but not terrible. My husband did them for me. After that, they realized that I was a strong responder - I had many follicles, and I was potentially at risk for ovarian hyperstimulation syndrome, an exaggerated response some women have from the process. My treatment was modified to make sure I would still have a successful cycle. Eventually, I was ready to trigger. I had a lot of pain, discomfort and nausea. I was also bloated and had a hard time eating. I was so ready for this to be done.
My egg retrieval was fairly easy. I was under anesthesia for about an hour and then went home. The first day or two I had a decent amount of pain, but it was bearable. By day 3, I was feeling normal, and by day 5 my bloating was gone. It felt great to be done. Twenty-seven of my eggs were retrieved: 13 were fertilized and eight were healthy enough to biopsy and send off for genetic sequencing. We were excited to learn that two of those embryos have a normal number of chromosomes and are BRCA1-negative. We don't plan to implant either of these embryos for about three years when I’m 33.
I feel so relieved that I went through this process and we now have two chances at becoming a full family. I was very fortunate to have the financial and medical support that I had in this process. I also found social support through the FORCE message boards, website, and a Facebook group for BRCA mutation carriers going through IVF with PGD. This process has many ups and downs, but I wouldn’t be where I am today without the support network I built. If you’re considering going through IVF with PGD, I encourage you to reach out to your support systems and build a network that will carry you through this journey.
